This blogpost was authored by Tim Robinson a co-principal investigator in two of our projects (#UrbanZoo and #ZooLink) and originally appeared on Cambribge Core Blog available at: http://blog.journals.cambridge.org/2017/01/24/confronting-the-rising-threat-of-antibiotic-resistance-in-livestock/
Resistance to antimicrobials is developing faster than ever before due to decades of abusing these important drugs. A ‘post-antibiotic’ world looms as a result, the consequences of which would be many people and farm animals sickening and dying of what, until now, have been preventable or treatable infections.
The good news is that the world is taking notice. On 21 September 2016, the United Nations General Assembly addressed this global challenge. At the UN headquarters in New York, member states reaffirmed their commitment to develop national action plans to stem and reduce the continuing rise in antimicrobial resistance (AMR). These action plans will be based on a Global Action Plan on Antimicrobial Resistance developed in 2015 by the World Health Organisation (WHO) together with the Food and Agriculture Organization (FAO) and the World Organisation for Animal Health (OIE)—the so called ‘Tripartite’. The aims of the Tripartite are first, to ensure that antimicrobial agents continue to be effective and useful to cure diseases in humans and animals; second, to promote prudent and responsible use of antimicrobial agents; and last, to ensure global access to medicines of good quality. Countries will be required to report on their progress in September 2018.
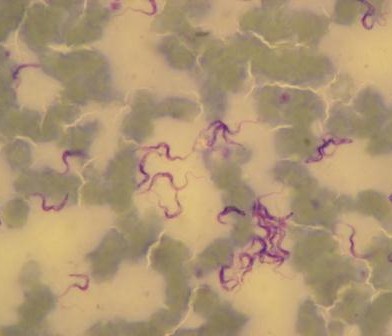
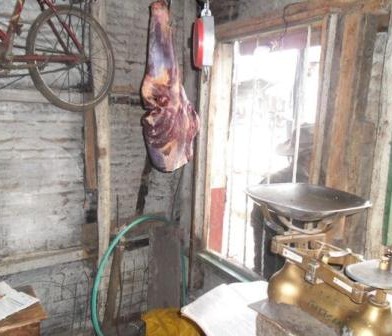
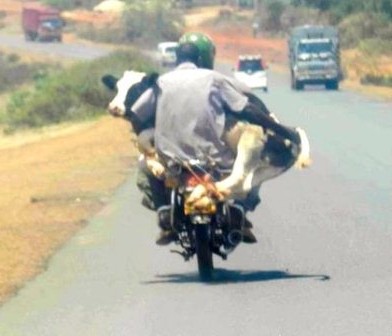
Addressing the rising threat of antimicrobial resistance requires a holistic and multisectoral ‘One Health’ approach, because of the interconnected roles played by animals, people and the environment in the evolution and spread of AMR. The potential role of the livestock sector in mitigating AMR in pathogens of medical as well as veterinary importance is critical. Livestock consume at least half of all antibiotics produced globally and there is a substantial and growing body of evidence linking antibiotic use in livestock production to the development of antibiotic resistance in disease-causing bacteria that pose major threats to public health.
It is widely held that the use of antibiotics in livestock production—in particular, to promote livestock growth and prevent disease, but also to treat disease—could be reduced considerably through improved production practices and other interventions. Robinson and colleagues propose interventions that can be made directly on farms; those that can help create enabling environments; and others that can raise awareness of the problem and ways to solve it.
The potential to reduce use of antibiotic drugs is particularly large in low- and middle-income countries where the use of antibiotics in livestock production is already high and is predicted to grow massively—if mitigation measures are not taken—in line with projected livestock sector growth. It is critical that this unique window of opportunity, with heightened public awareness and across-the-board political will so recently expressed, is harnessed to guide research and policy in AMR, and so to exploit fully the potential of livestock sector development to mitigate antibiotic resistance. The lives, health and well-being of people and livestock depend on our conserving these precious drugs as part of our arsenal against microbial infections.
The open access Opinion paper is published in animal: Antibiotic resistance: mitigation opportunities in livestock sector development
Authors: T. P. Robinson, D. P. Bu, J. Carrique-Mas, E. M. Fèvre, M. Gilbert, D. Grace, S. I. Hay, J. Jiwakanon, M. Kakkar, S. Kariuki, R. Laxminarayan, J. Lubroth, U. Magnusson, P. Thi Ngoc, T. P. Van Boeckel, M. E. J. Woolhouse











































You must be logged in to post a comment.