All you need to know about the novel 2019 coronavirus
All you need to know about the novel 2019 coronavirus
WHAT ARE CORONAVIRUSES?
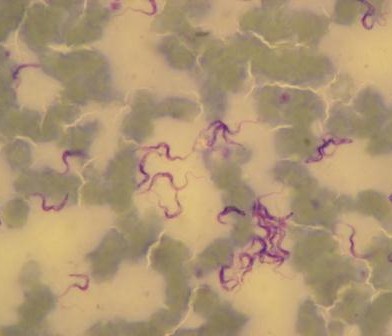
Coronaviruses are a large family of RNA (ribonucleic acid) viruses that are known to cause illness ranging from the common cold to more severe diseases such as Middle East Respiratory Syndrome (MERS) and Severe Acute Respiratory Syndrome (SARS). They are called coronaviruses because the virus particle exhibits a characteristic ‘corona’ (crown) of spike proteins around its lipid envelope.
Coronavirus infections are common in animals and humans. Some strains of CoV are zoonotic, meaning they can be transmitted between animals and humans, but many strains are not zoonotic.
In humans, coronaviruses can cause illness ranging from the common cold to more severe diseases such as Middle East Respiratory Syndrome (caused by MERS-CoV), and Severe Acute Respiratory Syndrome (caused by SARS-CoV). Detailed investigations demonstrate that SARS-CoV was transmitted from civets to humans, and MERS-CoV from dromedary camels to humans.

WHAT ARE THE SYMPTOMS OF THIS NOVEL CORONAVIRUS?
The symptoms can include a cough, possibly with a fever and shortness of breath. There are some early reports of non-respiratory symptoms, such as nausea, vomiting, or diarrhea. Many people recover within a few days. However, some people — especially the very young, elderly, or people who have a weakened immune system — may develop a more serious infection, such as bronchitis or pneumonia.

What is this novel coronavirus 2019?
The new Coronavirus 2019 is a zoonotic virus, which means it is a pathogen that spreads from one species to another, however it is unclear exactly what the origin of this virus is, but the genetic sequence is already being studied (https://www.sciencedaily.com/releases/2020/01/200131114748.htm)
A novel coronavirus (CoV) was identified in 2019 in Wuhan, China. This is a new coronavirus that has not been previously identified in humans.
On 31 December 2019, human cases of pneumonia of unknown etiology were reported in Wuhan City, Hubei Province of China. A coronavirus, named 2019-nCoV acute respiratory disease (2019-nCoV), was identified as the causative virus by Chinese authorities on 7 January 2020. Since then, human cases with travel history to Wuhan have been reported by several provinces in China and by a number of countries outside China.
For up to date information please consult the WHO website https://www.who.int/emergencies/diseases/novel-coronavirus-2019


How is this novel coronavirus treated?
Scientists are working hard to understand the virus, and Chinese health authorities have posted its full genome in international databases. Currently, there are no approved antivirals for this particular coronavirus, so treatment is supportive. For the sickest patients with this illness, specialized, aggressive care in an intensive care unit (ICU) can be lifesaving.

How can we combat new viruses?
Professor Eric Fevre explained the way to combat new viruses is being prepared and doing more routine and regular surveillance at places, which are a breeding ground for these viruses. “It’s very difficult to develop a drug or vaccine for something we don’t know about, so we always have to start the development process after those events have occurred,” he explained. But typically, it takes between four to five years to develop a vaccine for a new virus. Several groups are working on a vaccine right now, but there is no guarantee it will be ready before the end of the current outbreak.
What can we do to stay safe?
-
Avoiding unprotected contact with farm or wild animals.
-
People with symptoms of acute respiratory infection should practice cough etiquette (maintain distance, cover coughs and sneezes with disposable tissues or clothing, and wash hands).
-
Within healthcare facilities, enhance standard infection prevention and control practices in hospitals, especially in emergency departments
-
Based on currently available information, travel or trade restrictions are not recommended.

Are animals responsible for the 2019 novel coronavirus infections in people?
-
The source of this outbreak has yet to be confirmed but it could be any number of animal carriers from snakes to pigs.
-
Genetic sequence data reveals that 2019-nCoV is a close relative of other coronaviruses found circulating in Rhinolophus bat (Horseshoe Bat) populations.
-
There is suspicion that the 2019-nCoV may have had an animal source, but further investigations are required to confirm this.
-
Although there is suspicion that the initial introduction of 2019-nCoV to humans may have come from an animal source, the predominant route of subsequent transmission appears to be from human to human.
-
Ongoing investigations are important for identifying the animal source (including species) and establishing the potential role of an animal reservoir in this disease.


Why is One Health so important in situations involving emerging diseases such nCoV2019?
Stopping disease in humans by preventing disease in animals underpins the concept of “One Health”, an approach to public health that recognises the links between animals, people and planet. To bring this to bear and prevent similar outbreaks in the future, we need greater commitment, funding and research on these shared health threats.
By identifying disease threats and spread as early as possible, health authorities can take pre-emptive action, such as tighter biosecurity controls on farms or at food markets, or public awareness campaigns. By developing and using new and better treatments for animal disease, we can help stop their spread both among animal populations and among people.
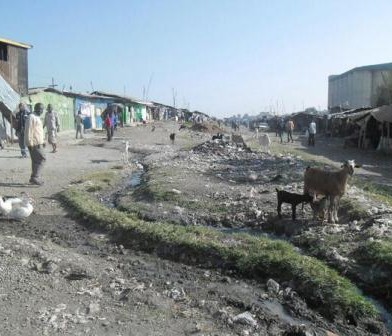
Where and how are new diseases likely to emerge?
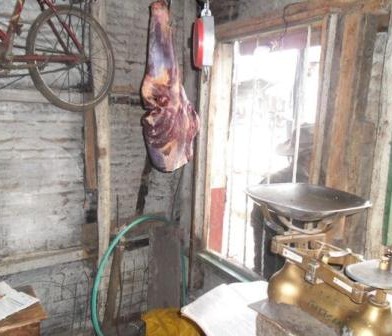
Our team lead, Eric Fevre, a professor of infectious diseases at the University of Liverpool, while speaking with ITV, outline that new diseases are likely to spring up in urban environments where humans have created very densely packed human populations, alongside a population of bats, rodents, birds, pets and other things living organisms. This creates an intense interaction and opportunities for pathogens to move from species to species. Other such environments, which are created as part of the economy or the way we live are slaughterhouses where individuals who work there are in intense contact not just with animals but with the different parts of the insides of animals or wet markets. Similarly, where animals are sold, cut up and cleaned and where there are a lot of people interacting with those individuals.
David Quammen, the author of “Spillover: Animal Infections and the Next Human Pandemic, in an opinion piece in the New York Times, “When people invade tropical forests and other wild landscapes, which harbor so many species of animals and plants — and within those creatures, there are so many unknown viruses. We cut the trees; we kill the animals or cage them and send them to markets. We disrupt ecosystems, and we shake viruses loose from their natural hosts. When that happens, they need a new host. Often, we are it.”
Other ways that disease emerge are current circumstances which include a perilous trade in wildlife for food, with supply chains stretching through Asia, Africa and to a lesser extent, the United States and elsewhere. That trade has now been outlawed in China, on a temporary basis; but it was outlawed also during SARS, then allowed to resume — with bats, civets, porcupines, turtles, bamboo rats, many kinds of birds and other animals piled together in markets such as the one in Wuhan. And one consequence of that abundance in human population, that power, and the consequent ecological disturbances is increasing viral exchanges — first from animal to human, then from human to human, sometimes on a pandemic scale.

What is the key take home message: Do not panic!
Given the current spread of this virus and the pace and complexity of international travel, the number of cases and deaths will likely to continue to climb. We should not panic, even though we are dealing with a serious and novel pathogen. Public health teams are assembling. Lessons learned from other serious viruses, such as SARS and MERS, will help. As more information becomes available, public health organizations like the World Health Organization (WHO) will be sharing key information and strategies worldwide.
Are there any precautions to take with live animals or animal products?
In accordance with advice offered by the World Health Organisation, as a general precaution, when visiting live animal markets, wet markets or animal product markets, general hygiene measures should be applied, including regular hand washing with soap and potable water after touching animals and animal products, avoiding touching eyes, nose or mouth with hands, and avoiding contact with sick animals or spoiled animal products. Any contact with other animals possibly living in the market (e.g., stray cats and dogs, rodents, birds, bats) should be strictly avoided. Attention should also be taken to avoid contact with potentially contaminated animal waste or fluids on the soil or structures of shops and market facilities.
Standard recommendations issued by the World Health Organisation to prevent infection spread include regular hand washing, covering mouth and nose when coughing and sneezing, and thoroughly cooking meat and eggs. Avoid close contact with anyone showing symptoms of respiratory illness such as coughing and sneezing. Raw meat, milk or animal organs should be handled with care, to avoid cross-contamination with uncooked foods, as per good food safety practices. Further recommendations from WHO can be consulted here: https://www.who.int/health-topics/coronavirus#
What are the Veterinary Authority’s international responsibilities in this event?
The detection of 2019-nCoV in animals meets the criteria for reporting to the OIE through WAHIS, in accordance with the OIE Terrestrial Animal Health Code as an emerging disease. Therefore, any detection of 2019-nCoV in an animal (including information about the species, diagnostic tests, and relevant epidemiological information) should be reported to the OIE.
It is important for Veterinary Authorities to remain informed and maintain close liaison with public health authorities and those responsible for wildlife, to ensure coherent and appropriate risk communication messages and risk management.
Effective biosecurity risk management and cooperation with inspection authorities should be maintained at borders.
What are key lessons we have learnt?
It may seem counter-intuitive, then, but with six out of 10 infectious diseases being zoonotic, one of the best ways to protect people from diseases like coronavirus is to first protect the health of animals. But recent novel cases of human coronavirus are just the latest reminder that we are too often missing the opportunity to act before new diseases emerge in people.
As David Quammen puts it, “We are faced with two mortal challenges, in the short term and the long term. Short term: We must do everything we can, with intelligence, calm and a full commitment of resources, to contain and extinguish this nCoV-2019 outbreak before it becomes, as it could, a devastating global pandemic. Long term: We must remember, when the dust settles, that nCoV-2019 was not a novel event or a misfortune that befell us. It was — it is — part of a pattern of choices that we humans are making.”
Further resources and references
Resources
- The World Health Organisation has a dedicated page for the Novel coronavirus (2019-nCoV) which provides information on how to protect yourself, Q&A, myth-busters, travel advice, situation reports and technical guidance https://www.who.int/emergencies/diseases/novel-coronavirus-2019
- OpenWHO: OpenWHO is WHO’s new interactive, web-based, knowledge-transfer platform offering online courses to improve the response to health emergencies. OpenWHO enables the Organization and its key partners to transfer life-saving knowledge to large numbers of frontline responders. https://openwho.org/ a course on Emerging respiratory viruses, including nCoV: methods for detection, prevention, response and control https://openwho.org/courses/introduction-to-ncov
- Here’s A Running List Of Disinformation Spreading About The Coronavirus https://www.buzzfeednews.com/article/janelytvynenko/coronavirus-disinformation-spread?utm_source=Nature%2BBriefing&utm_campaign=39e8741296-briefing-dy-20200128&utm_medium=email&utm_term=0_c9dfd39373-39e8741296-43314709
- Listen to the interview with our Principal Investigator, Prof Eric Fevre, as he speaks with the ITV News on, “Coronavirus: Where does it come from and how did it mutate to infect humans?” https://www.youtube.com/watch?v=clNkJGqTIJo&feature=youtu.be
References
- Coronavirus: How is a new virus born and where are they likely to emerge? By Natalia Jorquera. Posted on 1st February 2020 https://www.itv.com/news/2020-02-01/coronavirus-outbreak-how-is-new-virus-born-zoonotic-virus-wuhan-china-global-health-emergency/
- We Made the Coronavirus Epidemic posted on By David Quammen. Posted on 28th January 2020 https://www.nytimes.com/2020/01/28/opinion/coronavirus-china.html
- The new coronavirus: What we do — and don’t — know by Todd Ellerin, MD. Posted on 25 January 2020 https://www.health.harvard.edu/blog/the-new-coronavirus-what-we-do-and-dont-know-2020012518747
- China’s coronavirus outbreak proves we must pay closer attention to animal health by Carel Du Marchie Sarvaas. Posted on 24th January 2020 https://www.telegraph.co.uk/global-health/science-and-disease/chinas-coronavirus-outbreak-proves-must-pay-closer-attention/
- China coronavirus: how many papers have been published? by Emma Stoye on 30 January 2020 https://www.nature.com/articles/d41586-020-00253-8
- Questions and Answers on 2019-nCoV Acute Respiratory Disease by OIE https://www.oie.int/en/scientific-expertise/specific-information-and-recommendations/questions-and-answers-on-2019novel-coronavirus/
More resources on the novel coronavirus 2019
- Technical interim guidance for novel coronavirus, WHO: https://www.who.int/emergencies/diseases/novel-coronavirus-2019
- WHO travel advice for international travel and trade in relation to the outbreak of the novel coronavirus 2019-nCoV https://www.who.int/ith/2020-24-01-outbreak-of-Pneumonia-caused-by-new-coronavirus/en/
- Readiness is the key to detect, combat spread of the new coronavirus: https://www.who.int/southeastasia/news/detail/27-01-2020-readiness-is-the-key-to-detect-combatspread-of-the-new-coronavirus
- WHO’s Eastern Mediterranean Region scales up preparedness for novel coronavirus http://www.emro.who.int/media/news/whos-eastern-mediterranean-region-scales-up-preparedness-fornovel-coronavirus.html
- Press statements by KCDC (in Korean): https://www.cdc.go.kr/board/board.es?mid=a20501000000&bid=0015
- Wuhan Municipal Health Commission’s briefing on the pneumonia epidemic situation, (in Chinese): http://wjw.wuhan.gov.cn/front/web/list2nd/no/710
- Disease outbreak news, Novel Coronavirus: https://www.who.int/csr/don/en/
- Thailand Ministry of Public Health situation update on novel coronavirus (in Thai): https://ddc.moph.go.th/viralpneumonia/index.html
- Press statement by Ministry of Health, Labour and Welfare, Japan (in Japanese): https://www.mhlw.go.jp/stf/houdou/houdou_list_202001.html
- Notice sent out from Health and Food Safety Planning Division, Quarantine Station Operation Management Office (in Japanese): https://www.mhlw.go.jp/content/10900000/000582967.pdf
- Situation report by WHO on Novel Coronavirus (2019-nCoV) https://www.who.int/emergencies/diseases/novel-coronavirus-2019
- CDC press release. First Travel-related Case of 2019 Novel Coronavirus Detected in United States https://www.cdc.gov/media/releases/2020/p0121-novel-coronavirus-travel-case.html
- Hong Kong SAR Department of Health, Press Release https://www.info.gov.hk/gia/general/202001/23/P2020012300970.htm
- Epidemic Prevention Measures, Macau SAR Health Bureau https://www.ssm.gov.mo/apps1/PreventWuhanInfection/ch.aspx#clg17048
- Press release on 23 January 2020, Ministry of Health Singapore. https://www.moh.gov.sg/news-highlights/details/confirmed-imported-case-of-novel-coronavirusinfection-in-singapore-multi-ministry-taskforce-ramps-up-precautionary-measures
- CDC press release. Second Travel-related Case of 2019 Novel Coronavirus Detected in United States https://www.cdc.gov/media/releases/2020/p0124-second-travel-coronavirus.html
- New South Wales Government: Health: Coronavirus cases confirmed in NSW https://www.health.nsw.gov.au/news/Pages/20200125_03.aspx





 Human, food and environmental data are among the wide range of data collected within the
Human, food and environmental data are among the wide range of data collected within the 

 Article by
Article by 






































You must be logged in to post a comment.